How to Apply for Nursing Home Medicaid
Table of Content
- Medicaid Cost Sharing With Medicare
- Step 2: Assessing Medical Eligibility for Nursing Home Medicaid
- Medicare vs. Medicaid Roles in Nursing Home Care
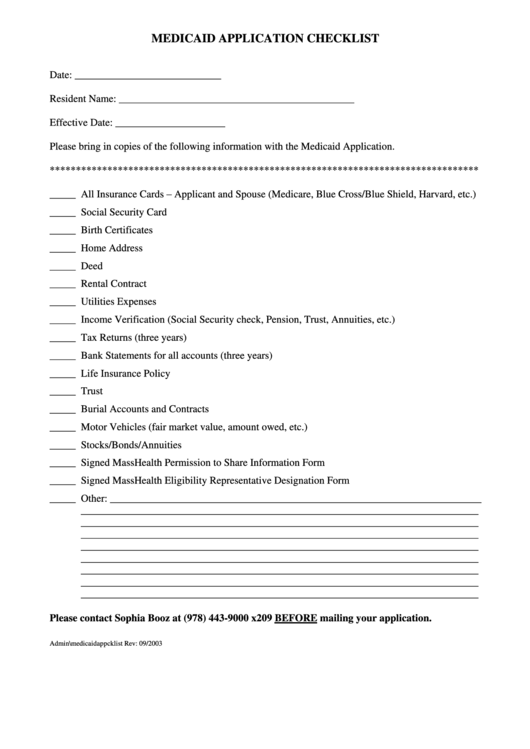
- Step 6: Complete and Submit Your Application for Nursing Home Medicaid
- Qualifying for Medicaid
- Whats The Difference Between Cdac And Cco In Elderly Waiver Programs
This includes a variety of long-term care benefits such as adult day care, doctor’s visits, skilled nursing care, in-home personal care, prescription assistance and transportation. ABD Medicaid beneficiaries qualify for these benefits and services one at a time, which is different from Nursing Home Medicaid, which makes all of its services immediately available for anyone who qualifies. Instead, ABD Medicaid recipients will be evaluated by the state to determine what kind of long-term care benefits they need and will receive. MI Health Link is a managed care program for Michigan residents who are eligible for both Medicaid and Medicare that combines the benefits of both programs into one plan.
Estate planning is the process of arranging for the transfer of your property after your death. It is important to consult with an experienced attorney or lawyer before making any decisions about Medicaid or estate planning. The laws surrounding Medicaid and estate planning are complicated and can vary from state to state.
Medicaid Cost Sharing With Medicare
The offers that appear in this table are from partnerships from which Investopedia receives compensation. Investopedia does not include all offers available in the marketplace. Let's look at how the economics work, and how Medicaid can be used to pay for a nursing home.
To be eligible for Michigan Medicaid, a person has to meet certain financial requirements and functional requirements. Another option is Miller Trusts or Qualified Income Trusts , which can get complicated but would be described basically as special accounts for someone to deposit income that put them over the Medicaid limit. Money in the trust would not count toward eligibility and would only be accessible by the applicant for specific purposes. The trust is managed by someone who is not the Medicaid applicant and can be used to pay for medical expenses not covered by Medicaid. In most states, Medicaid will not pay for a nursing home unless the individual has been admitted, but nursing homes won’t admit someone unless they have a means to pay. Some nursing homes will accept Medicaid-pending residents who are awaiting an approval letter from Medicaid.
Step 2: Assessing Medical Eligibility for Nursing Home Medicaid
MAGI replaced the former process for calculating Medicaid eligibility, which was based on the methodologies of the Aid to Families with Dependent Children program that ended in 1996. The MAGI-based methodology does not allow for income disregards that vary by state or by eligibility group and does not allow for an asset or resource test. If you do not meet all of these conditions, Medicare will not pay for your SNF care.

If the applicant meets the eligibility criteria, the Medicaid program must provide them with the assistance they require. A single applicant, aged 65 or older, is permitted up to $2,000 in countable assets to be eligible for nursing home Medicaid or a HCBS Waiver. An applicant’s home, home furnishings, personal items, and vehicle are generally exempt. However, remaining portions of COVID-19 stimulus checks are countable assets.
Medicare vs. Medicaid Roles in Nursing Home Care
Medicaid coverage is also highly unlikely, although it depends on individual state regulations. The Medicaid and Medicare programs are complex laws that make preparing for nursing home care and estate planning a challenge. However, it is important to understand the basics of these programs so you can plan accordingly.
In all 50 states and the District of Columbia, Medicaid will pay for nursing home care for persons who require that level of care and meet the program’s financial eligibility requirements. Readers should be aware that the financial requirements and the level of care requirements vary based on the state. Furthering the complexity is that the financial requirements change based on the marital status of the Medicaid beneficiary / applicant. For those who are eligible, Medicaid will pay for the complete cost of nursing home care, including room and board.
Medicaid and Nursing Homes: A Quick Guide to the Rules
Medicaid will pay for nursing home care on an ongoing, long term basis for however long that level of care is required, even if it is required for the remainder of one’s life. For married applicants with both spouses applying, the 2022 asset limit for nursing home coverage through Iowa Medicaid is $3,000 combined, and the income limit is $2,523 / month per applicant. For a married applicant with just one spouse applying, the 2022 asset limit is $2,000 for the applicant spouse and $137,400 for the non-applicant spouse, and the income limit is $2,523 / month for the applicant.

Mr. Biren also assists startups and nonprofits with optimization challenges through his innovative and novel use of synergies between tax, law, finance, science, and technology. Enrollees with high medical, behavioral or social needs should have access to a program of care management that includes the involvement of a multidisciplinary care team and the development of a written care plan. This is determined through a state assessment and reports from the applicant’s doctors and other relevant healthcare professionals. The functional, or medical, criteria for Nursing Home Medicaid in Michigan is needing a Nursing Facility Level of Care , which means the applicant requires the kind of full-time care that can only be provided in a nursing home.
Ways to spend down assets without violating this rule include purchasing an irrevocable funeral trust, paying off debt, and buying medical devices that are not covered by insurance. There are also several Medicaid planning strategies not mentioned on this page that can be used to help persons meet Medicaid’s asset limit. “Nursing Home Level of Care” may sound like an obvious care requirement, but each state defines “Nursing Home Level of Care” differently and there is considerable variation among the states.
This can be spent on personal items such as clothes, snacks, books, haircuts, cell phones, etc. It cannot be spent on any item that Medicaid covers, including hygiene basics like a toothbrush, soap, deodorant, razors and incontinence supplies, unless the Medicaid beneficiary wants a specific brand that is not covered by Michigan Medicaid. In this case, they could spend their personal needs allowance on the item. Individuals and couples who are over Medicaid’s income and / or asset limit, but still cannot afford their long-term care costs, can still qualify for Medicaid.
The table below is a generalized view of Medicaid eligibility for nursing home care. The “level of care” requirement for long-term care Medicaid differs based on the type of Medicaid program from which a senior is seeking assistance. For nursing home care or for home and community based services via a Medicaid Waiver, the level of care that is provided in a nursing home is generally required. For Aged, Blind and Disabled Medicaid programs that provide in-home care, often an applicant need only require limited personal care assistance.


Comments
Post a Comment